How Drugs Penetrate the Skin
Delivering drugs through the skin offers multiple advantages, including bypassing first-pass metabolism, reducing systemic side effects, and improving patient compliance. However, dermal penetration is a complex process governed by multiple physiological and physicochemical factors. Understanding these mechanisms is critical for optimizing transdermal drug delivery systems.
This blog post explores the key mechanisms of dermal drug penetration, factors influencing drug absorption, and evidence-based strategies to enhance transdermal delivery. Using the PAAS framework (problem-agnostic-amplify-solution), we’ll break down why some drugs struggle with skin penetration, the consequences of poor absorption, and how to improve drug delivery effectively.
The Challenge of Skin as a Barrier
The skin, particularly the stratum corneum, is the primary barrier that limits the penetration of drugs. Its role is to protect the body from external substances, preventing harmful agents from entering the bloodstream. While this defense mechanism is essential for survival, it also poses a significant challenge for transdermal drug delivery.
Unlike oral or injectable routes, transdermal delivery depends on passive diffusion through multiple layers of skin. This is not a simple process. Only a few drugs, such as nicotine, fentanyl, and scopolamine, have been successfully formulated into transdermal patches. Many potential transdermal drugs fail due to poor skin permeability.
The Consequences of Ineffective Dermal Penetration
When a drug fails to penetrate the skin effectively, several issues arise:
- Reduced efficacy: If the active ingredient doesn’t reach therapeutic levels in the bloodstream, it becomes ineffective.
- Wasted formulation efforts: Companies invest millions in formulating transdermal drugs that may not deliver results.
- Inconsistent dosing: Some drugs may penetrate unpredictably, leading to fluctuations in therapeutic outcomes.
- Patient dissatisfaction: If a transdermal product is ineffective, patients may switch to more invasive or inconvenient drug delivery methods.
Given these challenges, it becomes crucial to understand the mechanisms behind drug penetration and the factors that influence absorption.
Breaking Down the Science of Dermal Penetration
Mechanisms of Drug Penetration
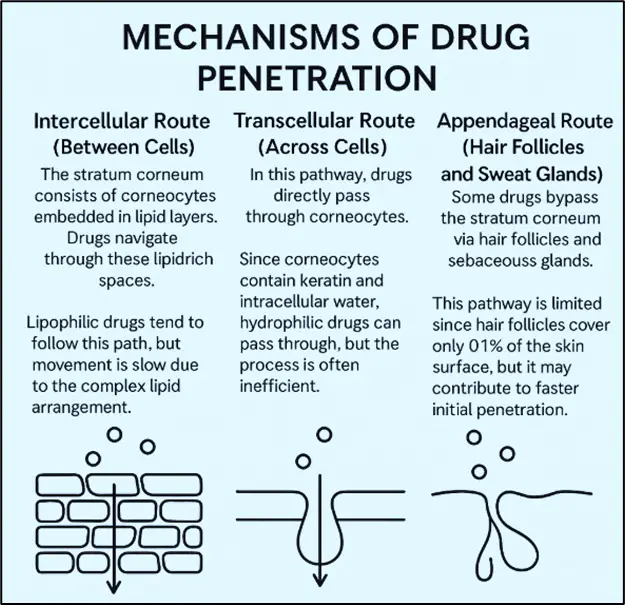
Drugs can penetrate the skin via three main pathways:
- Intercellular Route (Between Cells)
- The stratum corneum consists of corneocytes embedded in lipid layers. Drugs navigate through these lipid-rich spaces.
- Lipophilic drugs tend to follow this path, but movement is slow due to the complex lipid arrangement.
- Transcellular Route (Across Cells)
- In this pathway, drugs pass directly through corneocytes.
- Since corneocytes contain keratin and intracellular water, hydrophilic drugs can pass through, but the process is often inefficient.
- Appendageal Route (Hair Follicles and Sweat Glands)
- Some drugs bypass the stratum corneum via hair follicles and sebaceous glands.
- This pathway is limited since hair follicles cover only 0.1% of the skin surface, but it may contribute to faster initial penetration.
Factors Influencing Dermal Penetration
Several factors determine how well a drug penetrates the skin:
1. Physicochemical Properties of the Drug
- Molecular weight: Ideal transdermal drugs are below 500 Da. Larger molecules struggle to penetrate.
- Lipophilicity: Drugs with moderate lipophilicity (Log P between 1-3) show better skin absorption.
- pKa and ionization: Non-ionized drugs penetrate more efficiently, as the charged form has poor lipid solubility.
2. Formulation Factors
- Vehicles and solvents: Ethanol, propylene glycol, and dimethyl sulfoxide (DMSO) enhance solubility and penetration.
- Emulsions and nanoparticles: Liposomal and nanoemulsion formulations improve skin permeation.
3. Biological Factors
- Skin hydration: Hydrated skin absorbs drugs better than dry skin.
- Age and condition: Infants and elderly individuals have thinner skin, affecting absorption rates.
- Site of application: Areas like the face, underarms, and genitals have higher permeability than the back or limbs.
4. Enhancement Techniques
- Chemical enhancers: These alter the lipid bilayer to improve penetration.
- Physical methods: Techniques like microneedles, iontophoresis, and sonophoresis enhance drug delivery.
Optimizing Transdermal Drug Delivery
Evidence-Based Strategies
- Use of Permeation Enhancers
- Case Study: A study on diclofenac transdermal patches showed that using ethanol as a penetration enhancer significantly improved drug absorption (Patel et al., 2021).
- Formulation Optimization
- Research indicates that nanoparticles and liposomes enhance drug transport. A study on curcumin-loaded liposomes demonstrated a 3-fold increase in transdermal penetration compared to conventional formulations (Zhang et al., 2020).
- Physical Enhancement Technologies
- Microneedles: Used for delivering vaccines and insulin.
- Iontophoresis: An electrical method to push charged drugs through the skin.
- Ultrasound (Sonophoresis): Temporarily disrupts the stratum corneum, allowing large molecules to pass.
- Combining Approaches for Maximum Effect
- A 2022 study found that combining chemical enhancers with microneedles resulted in 10 times higher drug penetration than using enhancers alone (Singh et al., 2022).
Conclusion
Transdermal drug delivery presents significant challenges due to the skin’s natural barrier function. However, by understanding the mechanisms of dermal penetration and leveraging formulation advancements, penetration enhancers, and physical techniques, researchers and pharmaceutical companies can improve drug delivery efficacy.
The future of transdermal therapy lies in multi-modal approaches, including nanotechnology and microneedle-assisted delivery. By addressing the barriers methodically, we can expand the range of drugs that can be delivered through the skin, making treatments more effective and convenient.
The next step? More research into hybrid techniques that combine nanocarriers with advanced physical enhancement technologies. The field is evolving rapidly, and transdermal delivery may soon revolutionize how we administer a wide range of medications.
Frequently Asked Questions (FAQs)
1. What are the main challenges in transdermal drug delivery?
Answer: The primary challenge is overcoming the stratum corneum barrier to ensure adequate drug penetration.
2. Which drugs are most suitable for transdermal delivery?
Answer: Drugs with low molecular weight, moderate lipophilicity, and adequate potency are ideal candidates.
3. How can drug penetration through the skin be enhanced?
Answer: Techniques like microneedles, iontophoresis, chemical enhancers, and nanotechnology improve skin absorption.
4. Are transdermal drugs safer than oral medications?
Answer: They can be, as they bypass first-pass metabolism and reduce systemic side effects.
5. Can all drugs be formulated for transdermal delivery?
Answer: No, only certain drugs with appropriate physicochemical properties can be effectively delivered through the skin.