Ointments are semisolid preparations used for topical application, delivering drugs directly to the skin or mucous membranes. They are essential in treating dermatological conditions, infections, and pain management. Preparing ointments correctly ensures their effectiveness, safety, and stability.
This guide explains the methods of ointment preparation, types, essential ingredients, and quality control procedures to help pharmacists, researchers, and manufacturers ensure the best formulations.
Types of Ointments and Their Applications
Ointments are semisolid preparations applied to the skin or mucous membranes for therapeutic or protective purposes. They can be broadly classified based on function:
A. Medicated Ointments
Medicated ointments contain active pharmaceutical ingredients (APIs) that provide therapeutic effects. Some common types include:
- Antiseptic Ointments: Contain antimicrobial agents like povidone-iodine or neomycin to prevent infections.
- Analgesic Ointments: Include pain-relieving ingredients such as menthol, camphor, or capsaicin.
- Corticosteroid Ointments: Used for inflammatory conditions like eczema or psoriasis (e.g., hydrocortisone, betamethasone).
- Antifungal Ointments: Treat fungal infections like athlete’s foot (e.g., clotrimazole, miconazole).
- Antibiotic Ointments: Combat bacterial infections (e.g., Bacitracin, mupirocin).
B. Non-Medicated Ointments
These ointments act as protectants, emollients, or lubricants without active drug ingredients. Examples include:
- Emollient Ointments: Used to retain moisture in dry skin conditions (e.g., petroleum jelly, lanolin).
- Barrier Ointments: Form a protective layer on the skin to prevent irritation (e.g., zinc oxide for diaper rash).
Essential Ingredients in Ointment Formulations
Every ointment consists of key components that determine its consistency, stability, and therapeutic properties:
1. Active Pharmaceutical Ingredient (API)
- The medicinal component is responsible for the therapeutic effect.
- Examples: Antibiotics (mupirocin), antifungal agents (clotrimazole), and anti-inflammatory drugs (hydrocortisone).
2. Ointment Bases
The base provides the vehicle for drug delivery and influences absorption. They are classified into four main types:
- Oleaginous Bases (Hydrocarbon Bases) – They provide occlusion and are hydrophobic.
- Examples: Petrolatum, white ointment
- Absorption Bases – They can absorb water and form emulsions.
- Examples: Lanolin, wool fat
- Emulsion Bases – Provide hydration and improve drug release.
- Examples: Cold cream, hydrophilic ointment
- Water-Soluble Bases – They are Easily washable and leave no greasy residue.
- Example: Polyethylene glycol (PEG) bases
3. Stabilizers and Preservatives
- Prevent microbial contamination and increase shelf life.
- Examples: Parabens, benzyl alcohol, sorbic acid.
4. Penetration Enhancers
- Improve drug absorption through the skin.
- Examples: Ethanol, dimethyl sulfoxide (DMSO), surfactants.
5. Emulsifiers
- Maintain consistency in emulsion-based ointments.
- Examples: Sodium lauryl sulfate, cetyl alcohol.
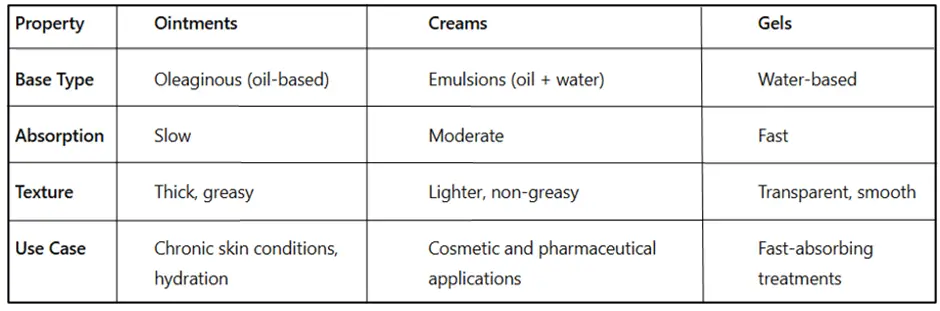
Key Differences Between Ointments, Creams, and Gels
Understanding the differences between ointments, creams, and gels helps in selecting the right formulation for specific conditions.
Methods of Ointment Preparation
There are three primary methods for preparing ointments, depending on their composition and intended use.
1. Fusion Method
- Used for bases that require melting before mixing.
- Common for oleaginous and absorption bases.
Steps:
- Heat oil-soluble components to 70-75°C.
- Heat aqueous components separately to the same temperature.
- Gradually mix the aqueous phase into the oil phase with continuous stirring.
- Allow the mixture to cool while stirring to maintain uniformity.
Example: Hydrophilic ointments, petrolatum-based ointments.
2. Incorporation Method
- Used for mixing powdered drugs or liquid APIs without heat.
- Suitable for heat-sensitive or volatile components.
Steps:
- Trituration – Mix a finely powdered drug with a small portion of the base.
- Levigating Agent – Add a suitable liquid (e.g., glycerin, mineral oil) to reduce particle size.
- Gradual Addition – Slowly incorporate the remaining ointment base using geometric dilution.
- Homogenization – Ensure even distribution of drug particles.
Example: Zinc oxide ointment, salicylic acid ointment.
3. Mechanical Incorporation Method
- Uses ointment mills, homogenizers, or planetary mixers for large-scale production.
- Ensures uniform particle dispersion and smooth texture.
Advanced Techniques in Ointment Formulation
With advancements in pharmaceutical technology, modern ointments now incorporate innovative drug delivery systems for better efficacy.
A. Use of Nanotechnology in Ointment Delivery
Nanotechnology has improved the delivery of APIs in ointments through:
- Nanoparticles: Enhance drug penetration through the skin barrier.
- Nanoemulsions: Improve solubility of poorly water-soluble drugs.
B. Liposomal and Transdermal Drug Delivery Advancements
Liposomal carriers help encapsulate drugs for controlled release, while transdermal ointments allow drugs to be absorbed directly into the bloodstream, bypassing the gastrointestinal tract.
Common Mistakes in Ointment Preparation and How to Avoid Them
Mistakes in ointment formulation can lead to reduced efficacy, contamination, and poor patient compliance.
A. Overheating Ingredients
- Heating sensitive ingredients beyond their melting points can degrade APIs.
- Solution: Use controlled-temperature heating and maintain phase separation in emulsions.
B. Incorrect pH Balance Affecting Drug Stability
- Some APIs degrade if the pH of the ointment base is too high or too low.
- Example: Salicylic acid becomes unstable in alkaline conditions.
- Solution: Use appropriate pH adjusters like citric acid or sodium hydroxide.
C. Contamination Risks During Manufacturing
- Microbial contamination can occur if proper sterilization methods are not used.
- Solution: Follow aseptic techniques, use preservatives, and conduct microbial testing.
Quality Control of Ointments
Ensuring safety, efficacy, and stability is critical in ointment formulation. Quality control tests include:
1. Physical Appearance
- The ointment should be smooth, uniform, and free from grittiness.
2. Spreadability Test
- Measures how easily the ointment spreads on the skin.
- Conducted using a spreadability apparatus or slide test.
3. pH Measurement
- Ensures compatibility with skin (~5.5) to prevent irritation.
4. Drug Content Uniformity
- Tests whether the active ingredient is evenly distributed.
- Uses HPLC (high-performance liquid chromatography) for accurate measurement.
5. Stability Testing
- Evaluate physical and chemical stability under different storage conditions.
- Common tests:
- Accelerated stability testing (40°C, 75% RH)
- Long-term stability studies
6. Microbial Testing
- Ensures the product is free from harmful contamination.
- Conducted using sterility tests and microbial limit tests.
7. Viscosity and Consistency
- Ensures the ointment has the right texture and flow properties.
- Measured using Brookfield viscometer.
Common Issues in Ointment Preparation and Their Solutions
Despite following standard procedures, some issues may arise during ointment formulation. Here’s how to address them:
| Issue | Cause | Solution |
| Ointment graininess | Improper particle size reduction | Use levigating agents and finer grinding |
| Phase separation | Incomplete emulsification | Use emulsifiers and control mixing temperature |
| Unstable API | Chemical degradation | Add antioxidants and store properly |
| Hard texture | Incorrect base selection | Modify base composition |
| Microbial contamination | Poor preservation | Use effective preservatives |
Advantages and Disadvantages of
Advantages of Ointments
- Provide prolonged drug action by forming a protective barrier.
- Reduce systemic side effects as the drug remains localized.
- Suitable for moisturizing and healing skin conditions.
Disadvantages of Ointments
- Greasy texture can be inconvenient for patients.
- Some ointments may cause skin irritation or allergies.
- Risk of microbial contamination due to prolonged use.
Conclusion
The preparation of ointments requires a scientific approach to achieve consistent quality and therapeutic effectiveness. Selecting the appropriate method (fusion or incorporation) and maintaining strict quality control measures are essential for safe and efficient drug delivery.
Future advancements in nanotechnology, bioactive delivery systems, and enhanced skin penetration techniques continue to improve ointment formulations, making them more effective for various dermatological and systemic treatments.
Frequently Asked Questions (FAQs)
1. What are the common bases used in ointment preparation?
Answer: The main bases include oleaginous (petrolatum), absorption (lanolin), emulsion (cold cream), and water-soluble (PEG-based) bases.
2. What is the best method for preparing ointments?
Answer: The fusion method is best for melting solid ingredients, while the incorporation method is suitable for heat-sensitive drugs.
3. Why are penetration enhancers used in ointments?
Answer: Penetration enhancers help drugs absorb more effectively through the skin, improving their therapeutic action.
4. How is the quality of an ointment ensured?
Answer: Quality is assessed through physical appearance, pH measurement, drug content uniformity, stability testing, and microbial contamination checks.
5. What are some common preservatives used in ointments?
Answer: Common preservatives include parabens, benzyl alcohol, and phenoxyethanol to prevent microbial growth.