Blood grouping is a classification of blood based on the presence or absence of certain antigens on the surface of red blood cells (RBCs). The two most important blood group systems are the ABO system and the Rh system. Understanding blood grouping is essential in various medical and transfusion-related scenarios to ensure safe blood transfusions and organ transplants. Here are the details of these blood group systems:
ABO Blood Group System
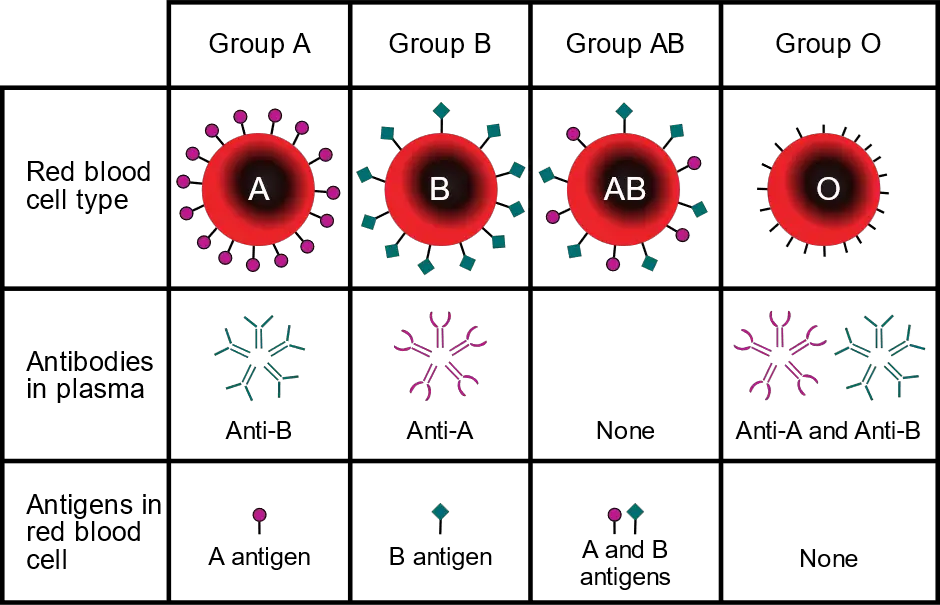
The ABO system categorizes blood into four main groups based on the presence or absence of two antigens, A and B, on the surface of red blood cells.
Blood can be classified into four main groups: A, B, AB, and O.
The Group A has A antigens on the surface of RBCs and anti-B antibodies in the plasma.
Group B has B antigens on RBCs and anti-A antibodies in the plasma.
The Group AB has both A and B antigens on RBCs and no anti-A or anti-B antibodies in the plasma.
Group O has no A or B antigens on RBCs but has both anti-A and anti-B antibodies in the plasma.
The compatibility of blood for transfusion follows the rule: Patients can receive blood from donors of the same or a compatible group, and individuals with type O negative blood are universal donors, while individuals with type AB positive blood are universal recipients.
Rh Blood Group System
The Rh (Rhesus) system categorizes blood into two groups based on the presence or absence of the Rh antigen (also known as the Rh factor or D antigen) on the surface of RBCs.
Individuals who have the Rh antigen on their RBCs are Rh-positive (+), while those who lack this antigen are Rh-negative (-).
The Rh factor is important during pregnancy, as Rh-negative mothers carrying an Rh-positive fetus may develop Rh incompatibility, leading to hemolytic disease of the newborn. To prevent this, Rh-negative mothers are typically given Rh immunoglobulin (RhIg) during pregnancy and after childbirth.
Other Blood Group Systems
In addition to the ABO and Rh systems, there are numerous other blood group systems, each characterized by the presence or absence of specific antigens on RBCs.
Examples of other blood group systems include the Kell system, Duffy system, Lewis system, and Kidd system, among others.
These systems are less commonly used in blood transfusions but can be relevant in cases of specific medical conditions and organ transplants.
Rh factor
The Rh factor, also known as the Rhesus factor, is a protein found on the surface of red blood cells. It is an important blood group antigen with significant clinical implications, particularly during pregnancy and transfusions. Here’s a note on Rh factors:
1. Rh Antigens:
– The Rh factor consists of a group of antigens, the most significant being RhD (Rh-positive) and RhCE (Rh-negative).
– If a person’s red blood cells have the RhD antigen, they are said to be Rh-positive. If the RhD antigen is absent, the person is Rh-negative.
– The RhD antigen is the most clinically relevant and primary focus when determining a person’s Rh status.
2. Rh Blood Typing:
– Blood is classified into different Rh blood groups, typically called Rh-positive (+) or Rh-negative (-).
– The most common blood types are A+, B+, O+, and AB+ (Rh-positive), while A-, B-, O-, and AB- are the corresponding Rh-negative blood types.
3. Significance of Rh Factor:
– Rh status is crucial for blood transfusions and pregnancies.
– In blood transfusions, matching the Rh type of the donor with the recipient’s blood to prevent transfusion reactions is essential.
– In pregnancy, Rh incompatibility can occur if an Rh-negative mother carries an Rh-positive fetus. This condition is known as Rh isoimmunization.
– If the mother’s immune system becomes sensitized to the Rh factor, it may produce antibodies against the Rh antigen, leading to hemolytic disease of the newborn (HDN) in subsequent pregnancies.
– To prevent Rh isoimmunization, Rh-negative pregnant women are often administered an injection of Rh immunoglobulin (RhoGAM) around the 28th week of pregnancy and within 72 hours after childbirth if the baby is Rh-positive. This treatment prevents the mother’s immune system from producing antibodies against the Rh factor.
4. Inheritance of Rh Factor:
– The Rh factor is inherited as a Mendelian dominant trait, which means that if a person inherits one Rh-positive allele from either parent, they will be Rh-positive.
– Rh-negative individuals have inherited two Rh-negative alleles (homozygous for Rh-negative).
– An Rh-positive individual may be either homozygous for Rh-positive (carrying two Rh-positive alleles) or heterozygous (carrying one Rh-positive and one Rh-negative allele).
5. Rh Factor and Blood Donation:
– Rh status is considered when individuals donate blood or receive blood transfusions. Matching Rh types is important in ensuring safe and compatible blood transfusions.
Understanding a person’s Rh status is essential for medical purposes, especially in pregnancy and transfusion medicine. It helps prevent complications that can arise due to Rh incompatibility, ensuring the safety of both the mother and the baby during pregnancy and the recipients and donors during blood transfusions.